Common paediatric hormonal conditions
Growth assessment is recommended in several conditions:
1. when your child is failing to thrive.
2. When your child grows on low percentiles which are different from the family pattern.
3. When a child is faltering growth (not growing well height wise).
4. When there is a change to growth pattern- slowing down or accelerating growth.
5. When you have concerns regarding the child’s possible adult height.
A condition in which a child is significantly overweight for his or her age and height. There are medical conditions, environmental factors, nutritional habits or hormonal imbalances that can cause elevated weight in a child.
All children with elevated body weight to height ratio should be screened for hormonal and metabolic conditions because childhood obesity is linked to increased risk to develop insulin resistance and diabetes, high blood pressure, elevated blood cholesterol and triglycerides levels.
Precocious puberty- Precocious puberty is when a child’s body begins developing secondary sexual maturation signs too early. When puberty begins before age 8 years in girls and before age 9 years in boys, it is considered precocious puberty
Delayed Puberty: Puberty that happens late is called delayed puberty. This means a child’s physical signs of sexual maturity don’t appear by age 12 years in girls or age 14 years in boys. This includes breast or testicle growth, pubic hair, and voice changes. These are known as secondary sexual characteristics.
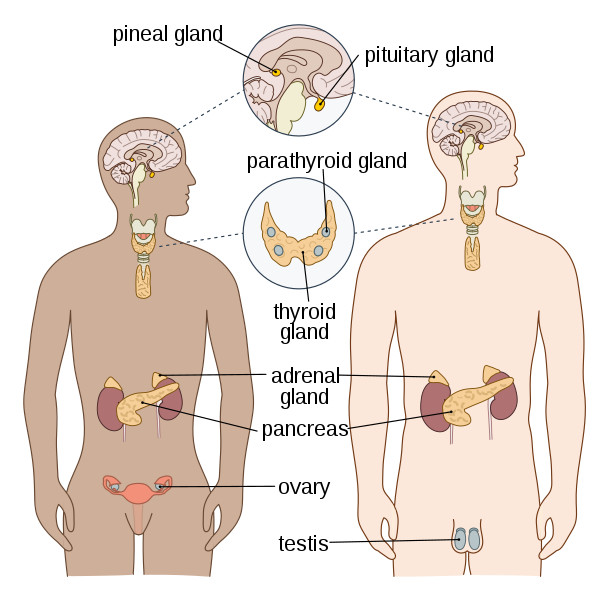
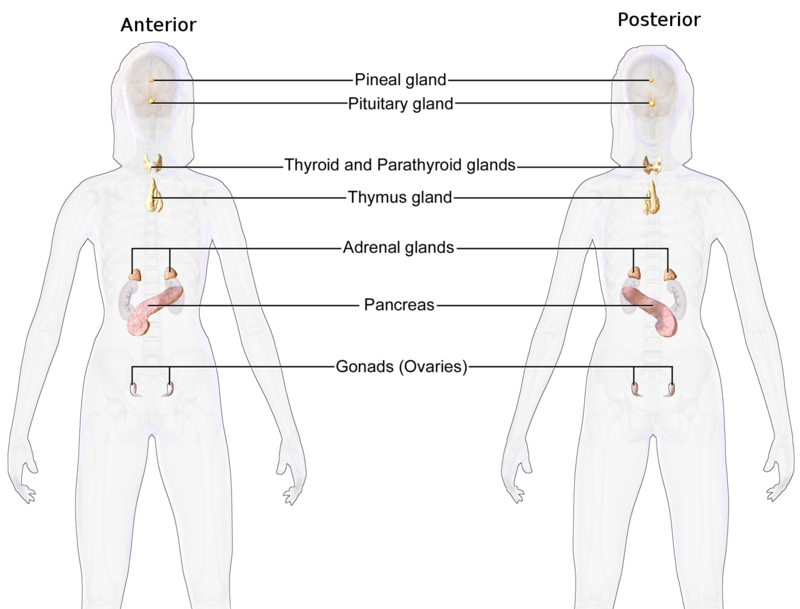
Thyroid is a small butterfly shaped gland that sits at the bottom of the neck. It regulate many of the body functions and metabolism.
Different thyroid conditions:
1. Congenital Hypothyroidism- when you are born with the lack of ability to produce thyroid hormones. This can be secondary to absent thyroid gland or the gland’s inability to produce hormones.
2. Acquired Hypothyroidism- this is a condition in which your thyroid gland doesn’t produce enough of the thyroid hormone. It can happen as part of an autoimmune process (where the body attacks and produces antibodies against it’s thyroid gland) or it can be secondary to other medical conditions.
3. Hyperthyroidism- when the thyroid gland losses control of the hormone production and produces too many thyroid hormones. This also can be secondary to autoimmune process or secondary to other medical conditions.
4. Thyroid nodules- which are lumps in the thyroid gland.
5. Goitre- enlargement of the thyroid gland, this can be secondary to autoimmune thyroiditis or other medical conditions.
Diabetes is a state when the blood glucose is elevated in an abnormal way. The body and the brain need glucose for energy and when there is impairment of glucose utilization and metabolism there are also clinical symptoms: lethargy, frequent urination, increased thirst, weight loss, inability to concentrate, increased hunger, loss of weight. There are several types of diabetes: Type 1 diabetes is the most common form in the paediatric population, when autoimmune antibodies destroy the pancreatic insulin producing cells (beta cells) leading to insulin deficiency and clinical symptoms. There are also other types of diabetes: Type 2 diabetes, monogenic diabetes (MODY), congenital diabetes, pancreatic insufficient diabetes (seen in conditions such as cystic fibrosis).
Treatment of diabetes is type dependant. Type 1 diabetes treatment is insulin, that can be given by multiple daily injections or insulin pumps. In the digital word we can perform zoom appointments with a paediatric endocrinologist, to review pump, CGM (continuous glucose monitors) or glucose sensors data upload and suggest changes to settings accordingly. Each child/adolescent receives a tailored plan that understands their individual needs, nutritional habits and general wellbeing.
Certain endocrine conditions cannot be diagnosed by a simple blood test. For example growth hormone deficiency- Growth hormone is a hormone secreted by the pituitary gland in the brain. Growth hormone promotes growth on all body organs and helps to gain height. Growth hormone is secreted in a pulsatile manner so it is impossible to catch the peak at a random blood test. A child that is not growing well and all other medical conditions were excluded may have growth hormone deficiency. To be diagnosed with growth hormone deficiency the child will need to be admitted for several hours is a specialized centre where he/she will have a cannula (an intra-venous line) inserted and blood growth hormone levels will be taken in time intervals after the child receives a medication that aims to stimulate growth hormone production by the pituitary gland.
There are other stimulation tests to diagnose: precocious puberty, delayed puberty, adrenal (another hormonal gland) insufficiency etc. The type of hormonal stimulation test should be recommended by a paediatric endocrinologist after carful assessment and only when indicated.
Gender dysphoria is a term that describes a sense of unease that a person may have because of a mismatch between their biological sex and their gender identity. This sense of unease or dissatisfaction may be so intense it can lead to depression and anxiety and have a harmful impact on daily life. Gender-affirming treatment includes giving hormonal medication that holistically attends to transgender people’s physical, mental, and social health needs and well-being while respectfully affirming their gender identity.
A hormonal disorder in a young female that can cause several clinical features: menstrual irregularity, excess hair growth (in a masculine way), acne and obesity. The cause of polycystic ovary syndrome isn’t well understood, but may involve a combination of genetic, environmental factors and certain medical conditions.
A paediatric endocrinologist will assess clinical signs and will recommend accordingly on investigations to identify the source of hormonal imbalance. Treatment will be adjusted according to the cause and clinical signs.
Adrenal abnormalities:
congenital adrenal hyperplasia- classical and non- classical. Other causes for adrenal insufficiency: such as Adrenal autoimmunity. Adrenal hypoplasia, prolonged steroid treatment.
Ambiguous genitalia-
Abnormal development of external reproductive organs including micropenis (small penile size), hypospadias, enlarged clitoris etc.
Hypoglycaemia–
low blood sugar.
Bone health:
problems with blood calcium or phosphate levels. Short stature with bone dysplasia. Low vitamin D levels.
Over production of hormones:
Gigantism (over productions of growth hormone).
Prolactinemia – Over production of prolactin hormone
Cushing syndrome – Over productions of cortisol.
Endocrine syndromes:
these are a group of genetic conditions that have hormonal manifestations. Turner syndrome, Noonan Syndrome, Klinefelter syndrome, Prader Willi, overgrowth syndromes etc.